Thursday 16th MayThe meeting started with Ed Poliness welcoming the participants and delivering the Acknowledgement of Country. This was followed by an ice-breaker based on a multi-group activity with different groups vying to solve a nine-letter word puzzle. The make-up of the groups then changed and the next challenge involved solving a numerical problem. Much fun was had by all with an opportunity to meet many colleagues. The keynote speaker was Dr John Kelly from NTGPE. John is a key proponent of remote supervision delivery through his work at Laynhapuy Homelands Aboriginal Corporation. He worked in the Homeland areas of NE Arnhem land, the ancestral land of the Yolngu people. He described being orientated by the nurse and the aboriginal cultural mentor to the area and to the work. John said he had to be honest and humble and be prepared to learn from his mistakes. His role provided health care and education to 12 Outstations. Living in the Outstations, aboriginal people are able to follow the traditional way of life. John said that these Outstations had no alcohol, petrol sniffing, gambling or suicide problems. The crime rate is minimal. The reason he gave for this low rate of social problems is that the aboriginal people in the Homelands are connected to the land. Difficulties he encountered included that English is the 3rd language, the need to understand men’s & women’s business, communicating issues when people may have “shame” and coping with a set of very different medical conditions such as rheumatic heart disease, strongyloidiasis etc. In addition, you needed to be very aware of the crocodiles. John found that valuable tools in these remote areas were Video-otoscopy, photography and video-recording, with appropriate permission, and using these recordings to get second opinions from specialist in distant centres. John’s technique for remote supervision is to arrange orientation for the registrar similar to his experience. He then sits in and observes and gives feedback on 30 to 40 consultations. He then has a clear of idea of the trainee’s capabilities. Remote supervision is provided by video-teleconference and previously he made himself continuously available for the registrar. Currently, he lives in Sydney and shares supervision with a supervisor who is on site 3 days a week. The internet has been a great advance for training purposes and he is able to do real time observation for ECTV’s. The limitations of this technique include difficulty in observing the clinical examination, demonstrating procedures and loss of internet connectivity. John supervises all levels of registrar who stay between six and twelve months. He has found that almost all the registrars have been very receptive to training but there has been the occasional registrar in difficulty, usually the registrar with preconceived ideas. An extensive discussion followed John’s presentation. When asked about funding for this supervision he advised that the funding came from the federal DOH. He not only supervises the registrars but also allied health personnel. There was a question about safety for the registrar and coping with emergency situations. John advised that the registrar is always accompanied by a nurse when they go to the Outstations. Training is provided for common emergency scenarios. The registrar’s progress is audited from the notes and documentation. There was a question about the relationship with the registrar and John pointed out that when they went out, he would take the 4-wheel-drive. The time together provided a good opportunity for discussion. During the discussion John said that even in the mainstream model where the registrar may feel remote even though they are in the next room. One of the GPT3 registrars present said that she was envious of the registrars supervised by John. Following morning tea, we had the choice of four concurrent Workshops:
In the afternoon there were six concurrent “World Café” discussions. Discussions from these will go towards a more in-depth discussion informing the direction of GPME at the September 2019 Workshop. The last session on Thursday included a choice of a further four concurrent Workshops:
Friday 17th MaySusan Tyler-Freer started the day with the Acknowledgment to Country. Graham Emblen (President) then introduced all the executive members. Lisa Fraser (Treasurer), Karen Aarons, Rebecca Lock, Rebecca Stewart and Greg Gladman. He said that currently GPME has a membership of 163. There were 92 participants at the meeting. He acknowledged the hard work of the education committee in organising the Workshop. The education committee includes Edmund Poliness (Chair), Denise Findlay, Rebecca Lock, Karen Savery, Susan Tyler-Freer and Hubert van Doorn. Next, Graham talked about GPME relationships with the Lead Medical Education Committee (LMEC), Australian College of Rural & Remote Medicine (ACRRM), Royal Australian College of General Practice (RACGP), General Practitioner Supervisors Australia (GPSA), the Department of Health (DOH) and the Registrar Training Organisation Network (RTON). GPME is independent of these organisations and is able to develop its own direction. The medical educator goal is to ensure that post-graduate medical education trains good quality general practitioners. He asked the participants to read through the constitution so that they understood the purpose of GPME. He also asked participants to share their ideas and passion through GPME Graham advised that the Sept Workshop would have four Masterclass sessions to discuss:
Graham talked about the challenges and the opportunities for medical educators presented by the funding change in the near future with funding being provided by the Colleges instead of the DOH. Hubert van Doorn, Jan Hanson and Neil then discussed those core values in medical education which won’t change, the transition, and what can be improved. There was a short presentation from Paul Grinzi from GPME Communication and IT Committee (ACIT). He explained GPME social media presence on Twitter, Web - https://www.gpme.asn.au/ and the closed Facebook page which is managed jointly with Rebecca Stewart. Paul then talked about the 2019 General Practitioner Training and Education Conference (GPTEC) and Rebecca Stewart advised that there are two free passes to be won to the conference in September. The first session of the morning consisted of the 2019 Med-XX Challenge where a number of educators role-played scenarios, gave tips using rhyming verse on improving Workshop sessions and used improvisational dance to take us through GP training journey. Presentations were as follows:
A further four concurrent Workshops followed morning tea:
For the writer, the Educational potential of ECTVs using video was of interest. In this session educators from NTGPE presented how they use video-recordings of consultations to improve consultation technique. In the discussion that followed the storage and destruction of the digital recording was explained. In addition, the medico-legal difficulties posed for using this technique in Victoria & NSW were explored. An important strength of this technique is the way the registrar can be brought back into the moment of a particular part of the consultation. A practical weakness is that sound quality can be poor. Next a role-playing method for training supervisors to use video-ECTV was presented and finally a role-play, consultation between registrar and patient was recorded and analysed. ACRRM for DumMEs was an interesting presentation of the curriculum and assessment process for ACRRM Fellowship. Because registrars are choosing ACRRM assessment more ME’s are involved with training towards the rural Fellowship. Another presentation of interest was, “MESP – the role of the Medical Educator Supervisor Portfolio”. In this session ME’s from GP Synergy, where there are 9 MESPs, presented the role of the MESP in their organisation. GP Synergy supports 1542 accredited practices with 2095 supervisors of which 1669 are in SE Sydney. There was a good discussion comparing the experience in different RTO’s. It was felt that each GPME Workshop should include a session for medical educators with the role of supervisor support. GP synergy have made their Supervisor Toolkit available to all supervisors. This can be found at: https://supervisortoolkit.gpsynergy.com.au/. To round off the session we discussed the following scenarios:
 Following afternoon tea there was a fun reflective activity with a gingerbread decorating activity. There was a great temptation to eat the art before the judging was finished. The Workshop finished at 3.30pm.
0 Comments
So you have been asked to see someone who you believe (or someone else believes) is not up to scratch in the way they are functioning as a doctor. How do you approach this situation? It can be one of the hardest parts of being a medical educator, and also one of the most rewarding. To be able to be effective in this area, there are a couple of things I believe you need. They are
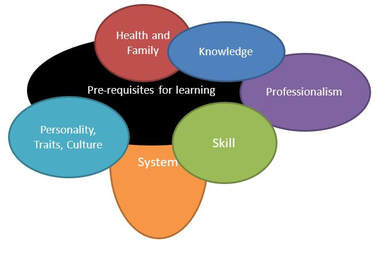
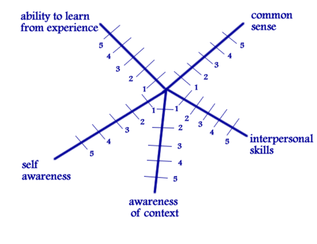
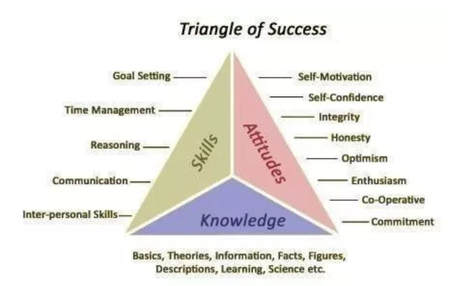
Recognition of the importance of the work you need to do. A doctor who is underperforming is one that can have significant impact on many people’s lives. Everyone they see is someone else’s mother/ father/ sister/ brother/child. They are all part of our community who deserve the best in health care. They deserve the best in health care they can receive. Failing to identify and support the doctor in improving means we are potentially committing that doctor’s patients to substandard care for the rest of that doctors career. An approach of Compassion. I believe that very few people get up in the morning and say “I am going to do a bad job today”. Most people approach their work with at least an intention to do things well. Most doctors who are underperforming want to do better. They may be unaware of what they are doing or aware but not sure how to change. This does not mean that we do not confront the person about their underperformance. An approach I have learnt to use over many years uses a term coined in a book by an American Paediatric Oncologist called “The anatomy of a lie” She used the word “carefrontation”- which is confrontation with care. You are challenging this doctor because you care about them and their patients, and so it is done with the intention to help. A sense of Curiosity We have heard the term “premature closure” in consultations. We can do the same when considering underperforming doctors. We have identified our pet problem doctors have, so that is the only problem they may have. Or this is the only thing we know how to fix, so that is the problem we will tackle. If you only have a hammer, then everything is a nail. Approaching the problem with curiosity, trying to understand what is going on here and considering as many possibilities or options that could be part of the problem helps in supporting the doctor toward change. A diagnostic framework. Below is a framework I have progressively modified over the years. I use if because it leads me into considering the best approach to remediation. This model considers core areas that impact on performance. Each of the areas may overlap and interact. Your role is to work out where the greatest point of leverage or point of influence may be. 1. Foundations for learning These are the fundamentals someone needs to have to learn. Without these, it is going to be very hard work for someone to improve. I have found that in particular, self awareness, awareness of context and ability to learn from experience are critical and can be hard to change. It is possible, but will take a lot of effort from both sides involved. Interpersonal skills can be learnt. I am not so sure about how people learn common sense, which seems to be not so common. Knowledge. This is a common area we blame for underperformance. We all have to have a background base knowledge level to function as a doctor. There is a significant level of assumed knowledge in all doctors. There will be some that have missed some core knowledge areas that can influence their performance. Often these are attempted to be hidden through embarrassment and so they need to be looked for in doctors who are not performing. As an educator, our role is not to make the person learn, but to help them find the most effective and efficient way to learn as well as guidance on what they need to learn. Skills. These are the individual behaviors that the doctor has to perform to be able to act out their roles in a meaningful and effective way. These are not just physical skills such as suturing and taking a blood pressure, but also communication skills and clinical reasoning skills. These are better observed by watching the doctor perform in their work, rather than self-reporting by the doctor. If they are deficient then we have to decide if this as a result of lack of the skill, lack of knowledge about the skills or is it that they don’t have a good role model to see how the skills are meant to work. If they have the skill but are not using it, is this because they do not perceive this as being valuable or part of their role or are they not motivated to use it, or do they not have the confidence to use the skill. Both knowledge and skills are areas that can be taught and learnt by anyone who has the pre-requisites for learning. Specific strategies are available for each different skill. Professionalism: Roles These are the clusters of behaviours that are expected to be learnt and used in the activity of being a GP. These include being a learner, a communicator, a diagnostician, an educator and others. Difficulties arise when: -
Interventions in relation to roles initially involve role clarification, or assistance in role conflicts. Where motivation is high, this can be a very rewarding area to work, as often dramatic change can be observed. Professionalism: Attitudes and Motivation This is the value placed on the activity and the behaviour by the doctor. How interested are they in working and behaving in the way they are being directed to. This is influenced by their belief in the value of the activity as well as by their confidence in their ability to carry the behaviour through. A doctor who is unmotivated will either openly reject your approaches or accept information with a tacit acceptance but with no intention of using the information. If this is the principal area driving poor performance, approaches used in motivational interviewing and behavior change become important, as this is in essence what we are seeking this doctor to do. Personality, Cultural Traits, Talents. These are the more inherent components of the person that influence their behaviour. They are things that they are born with, or develop as a result of their upbringing from family styles or cultural factors. This is the place where personality disorders may become evident. They tend to be less amenable to change. However this should not be a first label to apply. Other areas should be explored before attributing the difficult to this area. Systems. This is the structure in which we practice as a doctor. The computers used, the MBS, PBS, set-up of the practice and the systems and protocols that the practice uses to operate. There may be problems in this area that cause a doctor to underperform. There may be a lack of understanding about how the system works in a particular practice, or the system itself may be inappropriate or broken resulting in problems. As you may recognise, if this is the principal area, work may need to begin with the system around the doctor before on the doctor themselves. Health of individual and family. This important component needs to be always considered. The physical and mental health of the doctor and their family may have major ramifications in ability to perform and ability to change. If the doctor is suffering from some significant underlying emotional or physical illness then there performance will be significantly reduced. Also if the doctor has a significant family problem then this will impact on their performance. Acting on the other areas without identifying this area will result in sub-optimal change. All of the above factors interact to varying extents, hence the overlapping diagram. You may identify difficulties in a number of areas. Your approach then is to consider what are the priority areas and where might I have the greatest point of leverage, or the greatest potential impact. Also it is important to note that what is perceived to be a primary area may change through a remediation process, as with your curiosity, you discover other factors you were unaware of, or placed less value on in your initial assessment. Thus this process of assessment needs to be repeated as any remediation or support activities are instituted. Next steps after diagnosis Making a diagnosis is not the end of the assistance we need to provide to an underperforming doctor. To reinforce a point, the diagnostic framework used links to the different categories of interventions that could be implemented. To put it simply Knowledge: Strategies that enhance knowledge including learning styles, wrote learning, and relevant study techniques Skills: Skills training processes with demonstration, and rehearsal Systems: review of the systems to see if they are appropriate, understood or need modification Doctor and family health: requires external assessment and support Professionalism: this needs to use the skills in motivational interviewing and behaviour change. Personality, Cultural Traits, Talents: These may require a greater understanding and an assessment of whether there is the ability to influence or change these behaviours. Cultural awareness and cultural training may help. Self-awareness and awareness of context become critical for improvement in this area. Sometimes we may feel we have to find the one solution to a problem. It is like finding the man in the picture below. This may give you satisfaction, but will limit your consideration of the multiple and interacting factors that contribute to underperformance. Your role is to identify the range of factors and then identify the ones you can influence, choosing the ones that have the greatest point of leverage or impact on the presenting problem.
The work is often not easy. It is though very important, for that doctor and for all the patients they see for the rest of their career. Welcome to the first of our series of Medical Education Blogs. If you'd like to contribute, please let us know! This blog I have actually posted before and have since presented as a session to a group of MEs with much interest - so I thought it might be worthwhile to share more broadly. So AKT and KFP marks will be out soon and with that often comes the disappointment of an unexpected unsatisfactory result - and for MEs - the challenge of counselling the doctor. Human beings don’t like to fail. Doctors are terrible at it. It’s hard, especially when that failure is linked to self-esteem, professional image, and livelihood. But sometimes, the strong emotions that accompany failure, stop us from taking the time to consider why we may have had that outcome in the first place. Consequently, we habitually reattempt for success without reconsidering our approach – which can often lead to an unchanged outcome. I won’t pretend that I in any way understand how those that fail GP exams feel – I’ve only ever failed one exam in my life (my practical driving test – for not putting my seat-belt on) and I was devastated. But, I can offer some suggestions from my experience that might help them for the future. What do we do when a patient keeps coming back with the same unresolved symptoms? We usually try a few alternative treatments, perhaps increase a medication dose, whilst at the same time re-enquiring as to their initial symptoms, checking for red flags, and safety-netting. If they are still not getting better, we usually go right back to basics – retake the history again, re-examine, review the results of any investigations, perhaps read around the topic – and then reconsider what might be going wrong. If we still can’t work it out, we ask for a colleague’s insight. This approach works for doctors reattempting the exams as well. I’ve been working with doctors having difficulty with exams and in GP training for a long time, including researching and publishing on the topic. The reasons for having difficulty fall into three categories: Knowledge
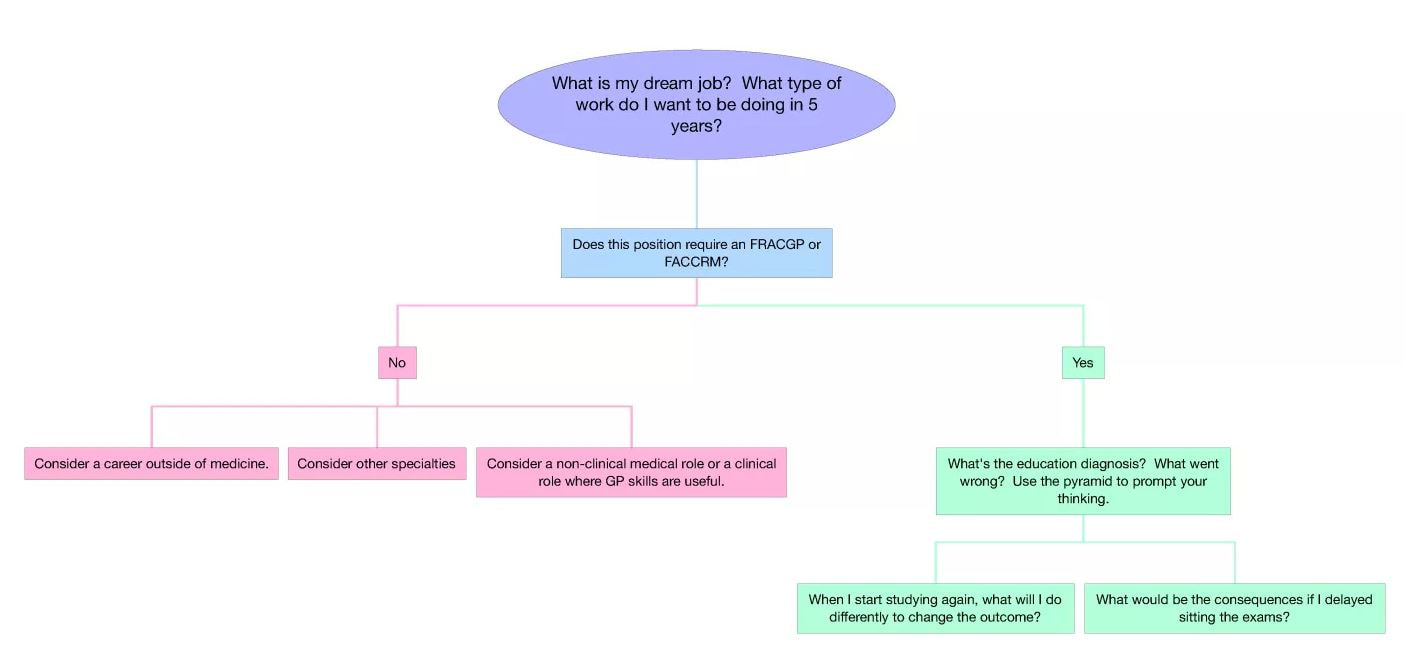
Reference Now I know that the last point above will have some of you thinking – and that’s what I had hoped. Gaining the FRACGP will make you a better GP, but you can still be a good doctor without it. Many of the doctor’s that I work with, have re-attempted the exams over and over, engaging in a new course of study between each attempt, and the outcome remains the same. They have the added burden of ‘study fatigue’ as they have been studying for many years, in addition to poor self-confidence and lack of self-belief due to constant failure. Re-attempting assessments needs to involve structured decision-making, so here’s what I suggest:
Make sure they know that if you keep doing things the same way, you will get the same result! After the recent AMEN Days, Cathy Regan (GP Synergy), who had spoken with a number of new MEs has set up a web blog particularly focussed on new MEs. Have a look at it at http://mededpurls.com/blog/
Anyone want to offer a comment, or send in a photo of what I gather was a great event. Sorry I missed it (Gary)
Erin Bryce from NTGPE is on the AMEN Communication and IT committee (known as ACIT).
She will be contacting the RTO reps to see if you want to share something about what you are doing in a blog. Erin can be contacted on [email protected] This topic is one of a few blogs that will be started on the AMEN website, which is more open than the facebook group.
Some of you won't have facebook, or haven't yet joined the AMEN Facebook page, but many of the 100 or so MEs who are on the facebook group have been excited by Rebecca Stewart's suggestion of a monthly online catchup with voluntary presenters on various topics related to Medical Education, including some focusing on new MEs and some for the more experienced MEs. This (says Rebecca) would build on the learnings and networking from AMEN as there's never enough time to catch up! Many have offered suggestions for topics and some have offered extra support to new MEs or an offer of a virtual meeting place. Rebecca liked the name MEME as it was a good acronym that somewhat fit the meaning of the word meme - "1 : an idea, belief or belief system, or pattern of behavior that spreads throughout a culture either vertically by cultural inheritance (as by parents to children) or horizontally by cultural acquisition (as by peers, information media, and entertainment media)" If you want to join Facebook, just email [email protected]. Some suggestions for topics so far have been (in no particular order) 1. basics for new MEs 2. Critical review of literature 3. Taking risks in teaching 4. The education diagnosis 5. Using iT to enhance learning 6. Planning learning 7. Curriculum design 8. Assessment 9. Feedback 10. Clinical Reasoning 11. Disruptive Learning/Teaching 12. Metacognition 13. Teaching IMG's |